2025 UK Surgical Workforce Census
Your insights are shaping a stronger and more sustainable workforce. By sharing your experiences, you help us deliver real change for patients and professionals across the UK. The 2025 UK Surgical Workforce Census builds on the 2023 Census findings, reflecting the priorities you raised and guiding our actions. Based on your feedback, we organised the findings into three pillars: productivity, training, and workforce sustainability, ensuring the results reflect what matters most to the surgical profession.
Your feedback and our actions
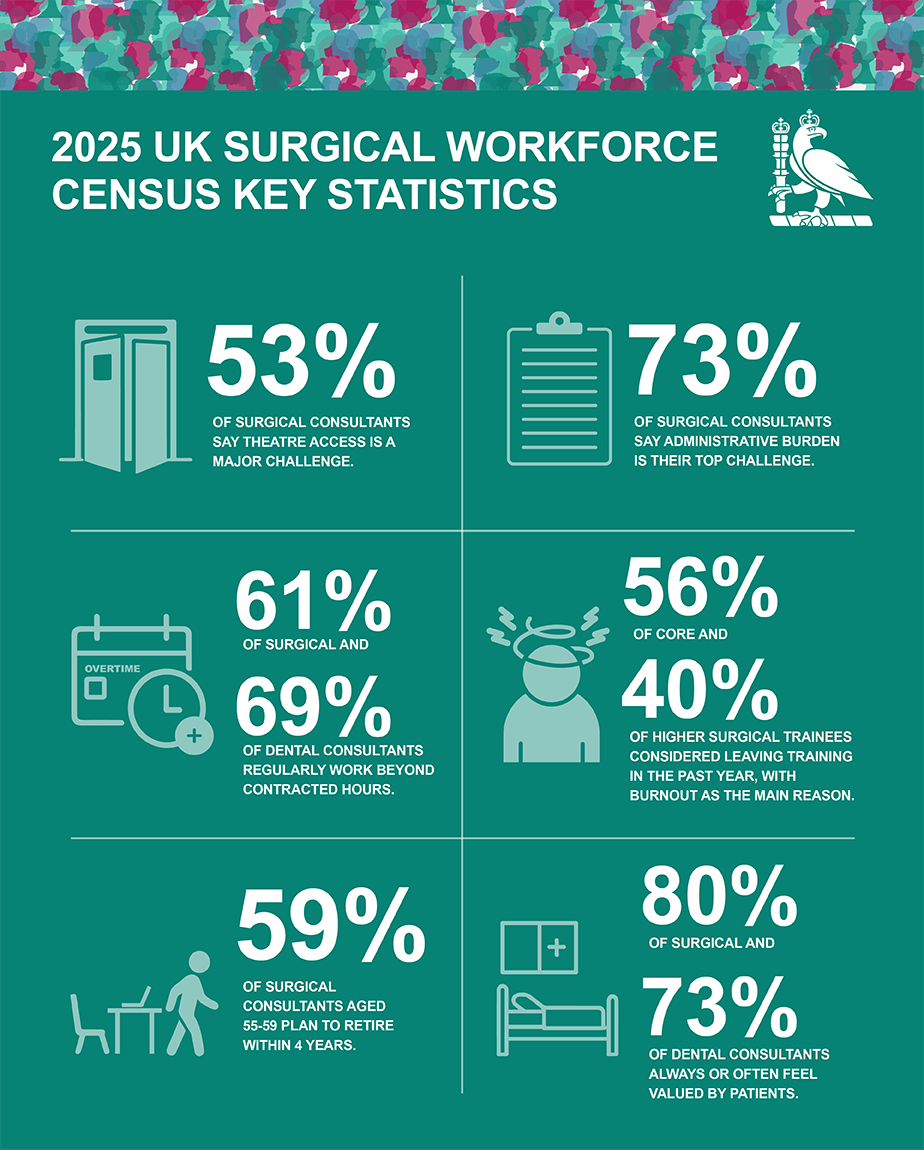
The 2025 Census highlights the dedication of the surgical workforce amid growing pressures. Productivity is constrained by restricted access to theatres, beds, and staff, alongside growing administrative burden and backlog pressures. Training opportunities are under significant pressure, with limited access to elective lists, rising burnout, and a growing risk of attrition among resident doctors. Workforce sustainability is challenged by persistent consultant vacancies and early retirement intentions. Conditions are challenging, but your feedback is driving action.
For detailed data, explore our toolkit.
Read our full report Advancing the Surgical Workforce: 2025 UK Surgical Workforce Census Report
Pillar 1: Productivity
What you told us:
- Outpatient and theatre pressures continue to constrain services: The increasing amount of administrative work was cited by 73% of surgical consultants, while 40% reported overbooked clinics and 37% noted that backlog pressures affected how they work.
- Theatre access remains a critical barrier: 53% of surgical consultants identified this as a major challenge, driven by lack of theatre space (73%), availability of theatre staff (59%), and bed availability (47%).
- Working beyond contracted hours is widespread: 61% of surgical and 69% of dental consultants always or frequently worked beyond their contracted hours. Additionally, 38% of surgical and 41% of dental consultants did not take their full annual leave entitlement in the past 12 months.
- The emergency workload is increasingly complex: 73% of surgical consultants and 64% of SAS surgeons reported having on-call commitments, with the most frequent pattern being 1:5 to 1:8. Consultants are managing both general and specialty-specific emergencies.
- Team stability is a concern: 41% of surgical consultants do not regularly work with the same anaesthetist(s). This is despite evidence that consistent theatre teams improve efficiency.
How we’re taking action:
- Developing job planning guidance specific to surgery, setting out best practice to ensure job plans for consultants, resident doctors, and SAS surgeons reflect real workload, reduce unnecessary administrative burden, and support flexibility.
- Publishing evidence on consultant working patterns through the Working Week of a Consultant Surgeon research, using findings to drive job planning reform.
- Calling for targeted government investment in surgical infrastructure, including operating theatres, beds, and staff, to deliver productivity targets and reduce waiting lists.
- Supporting outpatient transformation by promoting implementation of NHS England’s clinical and operational improvement guide.
- Building the evidence base for robotics and innovation through our RADAR network and Innovation Hub and advocating for capital, facilities, and training - so patients receive the right operation, at the right time, with the right technology.
Pillar 2: Training
What you told us:
- Theatre access is the biggest obstacle for resident doctors: 68% of core and 60% of higher surgical trainees reported limited access to elective lists, primarily due to emergency workload, theatre space, and staff shortages.
- Attrition risk is rising: 56% of core and 40% of higher surgical trainees considered leaving training in the past 12 months, with burnout cited as the main reason (65% core and 60% higher surgical trainees). These figures are higher among women, with 61% of core and 40% of higher surgical trainees reporting they have considered leaving.
- Dedicated time for training is a key area for improvement: 44% of resident doctors identified this as an issue. Reported frequency of supervision varied, with a small proportion noting that weekly meetings with their educational and clinical supervisors were limited.
- Exposure to the independent sector is inadequate: Just 10% of core and 7% of higher surgical trainees reported operating experience outside the NHS in the past 12 months.
How we’re taking action:
- Working with NHS England to update GIRFT accreditation guidance, ensuring that high-quality training requirements are explicit within surgical hubs.
- Collaborating with ASiT and surgical specialty training associations to call on NHS England and the Department of Health and Social Care (DHSC) to increase core and higher surgical training posts, targeting bottlenecks in progression and monitoring attrition rates.
- Collaborating with royal surgical colleges and wider medical education stakeholders to reform the curriculum to improve competence across the generality of a specialty, protect specialist roles, and reduce reliance on specialist centre rotations.
- We continue to participate in NHS England’s Training in Non-NHS Settings initiative, aiming to improve access to training opportunities in the independent sector for resident doctors.
Pillar 3: Sustainable workforce
What you told us:
- Consultant vacancies persist: 68% of surgical consultants reported new appointments in their NHS trust or health board in the past 12 months (42% replacement, 50% expansion), yet 39% reported unfilled consultant posts.
- Retirement intentions are concerning: 59% of surgical consultants aged 55–59 years plan to retire within four years, rising to 72% among female consultants. Note that there is variance in specialty data.
- Wellbeing is a key factor: 61% of surgical and 65% of dental consultants reported burnout and stress as major challenges.
- Workplace recognition is inconsistent: While most consultants feel valued by patients and colleagues, only 32% of surgical and 26% of dental consultants always or often feel valued by managers. Among resident doctors, just 11% reported always or often feeling valued by managers.
How we’re taking action:
- Accelerating progress on gender equity in surgery by strengthening the Women in Surgery (WinS) programme, expanding the mentoring pilot, supporting the Emerging Leaders programme, and ensuring female representation at Vice President level. We are also lobbying the government for fairer specialty place competition.
- Monitoring implementation of the NHS England Resident Doctor 10 Point Plan and national standards, advocating for better working conditions, ensuring all surgical teams have access to appropriate rest spaces and hot food.
- Driving full implementation of our SAS Strategy to integrate SAS and Locally Employed Doctors into the surgical workforce.
- Lobbying NHS England/DHSC, and employers to implement flexible and attractive early and late career pathways. This includes retire-and-return models, partial retirement, reduced on-call commitments, and portfolio careers, to retain senior surgeons and preserve clinical and educational capacity.
- Calling on stakeholders, including NHS England, DHSC, and regulators, to adopt the Turning the Tide recommendations, to eliminate sexual misconduct and create a safe, respectful working environment for all surgical staff.
Get involved
Help us turn evidence into action:
- Share the report and Toolkit with your local NHS trust medical director and ask how they are addressing these issues.
- Share on social media: Use our ready-made graphic for X, LinkedIn or Facebook.
Access workforce census data with our digital toolkit
The interactive census data toolkit is your digital companion to the 2025 report. Explore data independently, organised into key domains:
- Demographics
- Job plans
- Working conditions.
Each section includes filters so you can refine and review data that matters most to you. Navigation guidance is included to help you make the most of the toolkit.
Please note: the toolkit is best viewed in full screen and on desktop.
Explore more
Read the 2025 UK Surgical Workforce Census Report
Read the 2023 UK Surgical Workforce Census Report
Contact us
For further information please contact census@rcseng.ac.uk.
